When we talk about the end of a patient's life, difficult questions arise. Are we as a society ready for this sensitive issue? How do we balance the right to self-determination with our moral obligation to reduce suffering? This article looks at the complexity of euthanasia and assisted suicide in the Netherlands. We seek answers to these essential questions.

Key points
- We examine the definition and different forms of euthanasia.
- We discuss the legal aspects and the due diligence requirements around euthanasia in the Netherlands.
- We explore the ethical issues involved in the life-ending process.
- We look at the practical experiences of physicians and patients.
- We discuss assisted suicide and the role of government and health care providers.
- We explore alternatives for euthanasia, such as palliative care.
The question that can affect us all is: What makes euthanasia and assisted suicide so difficult? Delve deeper into these challenging topics. Discover the nuances in an issue that affects us all.
What is euthanasia?
Euthanasia is a topic of much debate. But what does euthanasia actually mean? It is the termination of life by a physician at the patient's request. This is done to end intolerable suffering. It can be done in several ways, which we will explain in more detail below.
Definition of euthanasia
Definition of euthanasia is the intentional termination of life by a physician. This is done at the express request of the patient. The patient must be in a hopeless and unbearable situation. Euthanasia is thus a conscious decision made by the patient himself, which is performed by a physician.
Forms of euthanasia
There are several forms of euthanasia:
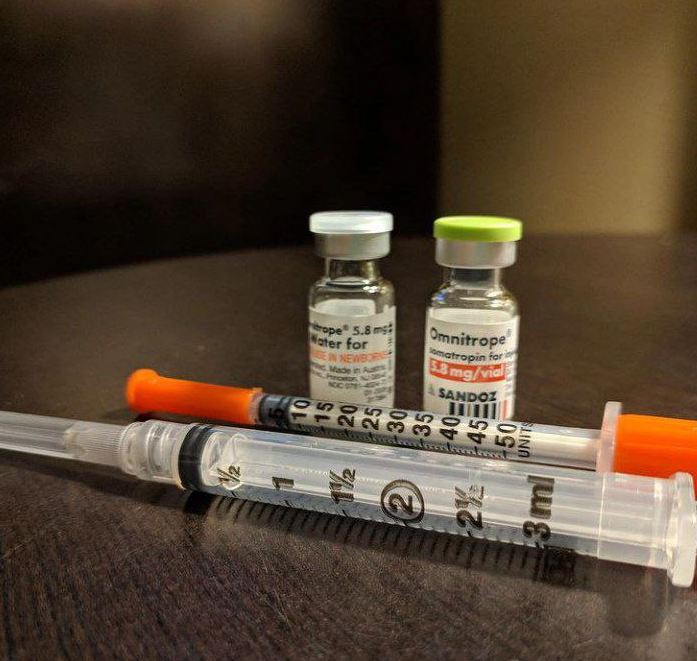
- Active euthanasia: the physician actively takes measures to end the patient's life. This can be done by lethal injection.
- Passive euthanasia: the doctor decides to stop continuing life-extending treatments. As a result, the patient dies.
- Voluntary euthanasia: euthanasia takes place at the express request of the patient himself.
All of these forms of euthanasia touch on complex ethical issues. We will discuss these later.
Euthanasia in the Netherlands
In the Netherlands, euthanasia is a recognized part of health care. Euthanasia legislation is very progressive and allows patients to end their suffering under certain conditions. This policy is the result of years of discussions about ethics and law.
The Dutch Euthanasia Act, in effect since 2002, states that euthanasia is permitted under certain conditions. Doctors may perform euthanasia if the suffering is unbearable and the patient wants it. They must also act carefully and report the euthanasia.
Although legislation is strict, euthanasia is a complex issue in the Netherlands. Many support the policy, but there is also criticism. Especially on the broadening of the law in 2002 to include psychological suffering. The debate over euthanasia in the Netherlands is ongoing.
| Key points euthanasia in the Netherlands | Explanation |
|---|---|
| Euthanasia legislation | The Euthanasia Act in the Netherlands is one of the most progressive in the world, allowing euthanasia under strict conditions. |
| Care requirements | Doctors must act carefully, meet conditions such as hopeless and unbearable suffering, and report the euthanasia to a review board. |
| Public opinion | The majority of Dutch people support the euthanasia policy, but there is also criticism, especially of its broadening to psychological suffering. |
Euthanasia legislation in the Netherlands is a complex and sensitive issue. It is a balancing act between individual autonomy and careful procedures. Euthanasia in the Netherlands is an important issue that deserves attention.
The legal aspects of euthanasia
The legal procedures surrounding euthanasia in the Netherlands are complicated. They require diligence. Doctors who wish to practice euthanasia must follow specific legal requirements. These requirements are essential to ensure the legality of euthanasia.
Euthanasia procedure in the Netherlands
The euthanasia process in the Netherlands has several steps. First, the doctor must be convinced of the patient's hopeless and unbearable suffering. Then the doctor informs the patient about his or her situation and options.
The doctor should also consult a second, independent physician for a second opinion.
Care requirements for euthanasia
- The patient must want euthanasia voluntarily and deliberately.
- The patient's suffering must be hopeless and unbearable.
- The physician must properly inform the patient of the situation and options.
- The physician must receive advice from at least one other independent physician.
- Euthanasia must be performed carefully.
If these requirements are met, the doctor can give euthanasia without criminal consequences. The regional review board assesses whether the doctor has complied with the legal procedures euthanasia and due diligence euthanasia has acted.

Physicians should be well aware of these legal procedures euthanasia and due diligence euthanasia. This allows them to perform euthanasia lawfully and carefully.
The ethical issues surrounding euthanasia
Euthanasia is a complex and sensitive subject. It deals with the fundamental right to life. On the one hand, this is inalienable, but on the other hand, human suffering can be so bad that euthanasia is seen as a solution.
The moral aspects of euthanasia are very important. It questions how much power a physician may have over a patient's end of life. Where is the line between autonomy and protecting the right to life? And what is the role of society in this matter?
- The right to life versus the right to self-determination
- The role and responsibility of the physician
- Social impact and responsibility
| Ethical dilemma | Arguments for | Arguments against |
|---|---|---|
| Right to life | No one has the right to decide over the life of another. | In extreme cases, suffering may be so unbearable that the right to self-determination prevails. |
| Role of the physician | Doctors have a duty to protect life and relieve suffering. | Physicians can also play a role in respecting the patient's wishes. |
| Social responsibility | Society has a duty to protect vulnerable citizens. | Society must also allow for individual end-of-life choices. |
The dilemmas surrounding euthanasia show that it is a complex issue. Different interests and values must be weighed against each other. It is a subject that challenges us to reach careful decisions.

"Euthanasia is one of the most difficult moral issues we face. It goes to the heart of our human existence and raises fundamental questions about the value and limits of life."
Euthanasia in practice
Euthanasia is a complex and sensitive subject. It is important to highlight its practical side. By sharing doctors' and patients' experiences, we gain a better understanding.
Experiences of doctors
Doctors who perform euthanasia feel a great responsibility. According to research among Dutch doctors, most indicate that they proceed carefully and according to legal procedures. They find it important to communicate well with the patient. It is also essential to palliative care offer and involve loved ones in the decision-making process.
"Euthanasia for me is the last resort, when all other options have been exhausted. It is a difficult decision, but also a way to give someone the dignity they deserve."
Patient experiences
Patients often choose euthanasia to maintain control over their end of life. Surveys show that many patients are satisfied with the care and support they receive. However, some worry about possible pressure from loved ones or doctors.
- Good communication and a listening ear are essential for patients.
- Patients want to feel heard and understood in their choice of euthanasia.
- Trust in the physician and the care process is key.
The experiences of both doctors and patients give us a better picture of euthanasia in practice. It shows that it can be a complex but sometimes necessary process for someone to die with dignity.

Assistance with suicide
In addition to euthanasia, there is also "assisted suicide." This means that a person chooses to stop living and receives help from a physician or health care provider. This topic is complex and sensitive, with many legal and ethical issues.
What is assisted suicide?
Assistance with suicide is different from euthanasia. In euthanasia, the doctor does the work of ending life. In assisted suicide the patient does this himself, but gets help from a physician.
In the Netherlands, the rules for assisted suicide are different from those for euthanasia. Euthanasia is sometimes allowed, but assisted suicide is usually prohibited. Still, it sometimes happens that doctors do help.
The discussion of assisted suicide raises major ethical questions. Consider the freedom of the patient, the role of the physician and the responsibility of society. It is a subject in which many interests are weighed against each other.
- Assisted suicide differs from euthanasia in that the patient makes the decision and acts on his or her own.
- The legal aspects around assisted suicide are different from euthanasia.
- Assisted suicide raises ethical questions about autonomy, the role of the physician and the responsibility of society.
The role of government and health care providers
The government and health care providers are very important in the euthanasia debate in the Netherlands. The government makes the government policy euthanasia and provides guidelines and laws. Health care providers, such as doctors and nurses, perform euthanasia.
The government checks that euthanasia is done properly. They look to see if all the rules are followed. This helps protect patients and maintain confidence in the law.
Health care providers, especially doctors, are very important in euthanasia. They have to check if a patient really meets the criteria. They inform and guide the patient and perform euthanasia if it is right.
Cooperation between government and health care providers is essential. They make sure euthanasia is good and accessible. This is important for patients.
"The government and health care providers must work together to ensure a careful and humane euthanasia policy that puts patients' autonomy and dignity at the center."
Alternatives to euthanasia
For many people, euthanasia is a complicated and sensitive subject. Fortunately, there are other ways to deal with the end of life. Such as palliative care and pain management. These alternatives provide support and comfort for patients and their loved ones.
Thus, they do not have to choose euthanasia. Palliative care focuses on relieving symptoms. It provides comfort for terminally ill patients.
This can be done through pain management, psychological support and practical help. This allows patients to spend their last phase of life with dignity.
Meaningfulness, spirituality and the involvement of loved ones are also important. By emphasizing these aspects, we can do justice to patients' individual needs and wishes.
FAQ
What is the definition of euthanasia?
Euthanasia means that a doctor ends a patient's life at their request. This can be done in several ways, such as actively or passively.
What are the different forms of euthanasia?
The forms of euthanasia are: - Active: a drug is given to end life - Passive: a treatment is stopped or not started, causing death - Voluntary: the patient himself requests euthanasia
How is euthanasia regulated in the Netherlands?
In the Netherlands, euthanasia is permitted under certain conditions. Doctors must meet due diligence requirements and report the euthanasia. The legislation is laid down in the Act on Testing life termination on request and assisted suicide.
What are the legal procedures for euthanasia in the Netherlands?
For euthanasia in the Netherlands, there are procedures. Doctors must determine the patient's suffering and obtain a second opinion. They must also report the euthanasia to a regional review board.
What are the ethical dilemmas surrounding euthanasia?
There are ethical issues in euthanasia, such as the right to life and the role of the physician. There is also debate about the balance between autonomy and protection of vulnerable groups.
How do doctors and patients deal with euthanasia in practice?
Euthanasia is a careful and emotional process. Physicians struggle with their role, while patients and loved ones want to manage their end of life.
What is the difference between euthanasia and assisted suicide?
The main difference is that in euthanasia, the doctor does the life-ending act. In assisted suicide, the patient does it himself, but receives help from a physician.
What is the role of government and health care providers around euthanasia?
The government regulates euthanasia in the Netherlands. Healthcare providers, especially doctors, must comply with due diligence and report euthanasia. They are also important in counseling patients and their loved ones.
What are the alternatives to euthanasia?
Alternatives include palliative care and pain management. These allow patients to suffer less without ending life. This allows them to have a dignified end.